Unveiling the Therapeutic Potential of Abaloparatide in Treating Periodontal Dehiscence
Researchers demonstrate that intraoral administration of abaloparatide combined with orthodontic force supports alveolar bone thickening
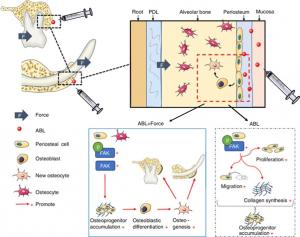
CHINA, September 19, 2025 /EINPresswire.com/ -- Alveolar bone defects can cause periodontal dehiscence, leading to exposure of dental roots, recession of gums, and increased tooth sensitivity. In a new study, researchers have evaluated the therapeutic potential of abaloparatide (ABL), a synthetic analog of human parathyroid hormone-related protein(PTHrP), in alleviating periodontal dehiscence. Utilizing rat models undergoing orthodontic tooth movement, they demonstrate that submucosal injection of ABL induces alveolar bone formation through a focal adhesion kinase(FAK)-driven mechanism.Alveolar bone, the specialized tissue within the jawbone, plays an important role in periodontal health. This tissue has a remarkable capacity of bone remodeling in response to mechanical stimuli like mastication force during chewing or applied orthodontic force. Defects in the alveolar bone can cause periodontal dehiscence, a condition where the roots of the tooth are exposed, leading to gingival recession and increased tooth sensitivity. Moreover, low alveolar bone thickness is associated with a high risk of dehiscence during orthodontic tooth movement, necessitating bone grafting surgeries to alleviate this detrimental side effect.
Recent studies indicate that abaloparatide (ABL), a synthetic analog of human PTHrP and an osteoporosis medication, may enhance alveolar bone formation. However, ABL’s efficacy and the underlying mechanism of augmenting alveolar bone formation remains unclear. To address this gap, a team of scientists comprising Professor Yu Li from the Department of Orthodontics, Sichuan University, China, and Professor Quan Yuan from the Department of Oral Implantology, Sichuan University, conducted a new study. Their findings published online in Volume 17 of the International Journal of Oral Science on September 02, 2025, reveal insights into the therapeutic potential and the biological mechanism of the ABL-mediated endogenous alveolar bone augmentation.
“Despite our previous study demonstrating the potential of ABL to augment alveolar bone, two critical questions remained unanswered. First, can a local injection of ABL induce alveolar bone formation? Second, can the results obtained for the labial (front teeth) area translate similarly to the buccal (back teeth) alveolar bone of rat molars? This inspired our research group to conduct an in-depth study using various animal models.” says Prof. Li, explaining the motivation behind the present study.
Initially, the researchers developed a labial movement (LM) model by utilizing an inclined bite splint to labialize the mandibular incisors of the rats. ABL was locally administered through an intraoral submucosal injection, either in combination with the LM force or alone. After 2 weeks of treatment, micro-CT showed that the labial alveolar bone thickness was significantly increased in the ABL + LM group, but not in the ABL-alone group. HE staining, a technique to visualize tissue structures under a microscope, revealed significantly increased alveolar bone tissue width and periosteal cells in the ABL + LM group. Additional analyses indicated that osteocalcin (OCN), a key protein involved in bone formation, was upregulated only in the ABL + LM group.
To verify if ABL’s effect was unique and limited to the rat labial area, the scientists developed a buccal movement (BM) model using a maxillary expansion device to apply force on the maxillary molars. Following a 2-week exposure to ABL, they assessed the thickness of buccal alveolar bone in each group. In line with the LM model observations, the ABL + BM group displayed increased thickness at the crest level. At the mid-ridge level, the ABL-alone group also resulted in enhanced alveolar bone thickness.
The research team then paid their attention to identifying the underlying mechanism of ABL-induced alveolar bone formation. Through mRNA sequencing analysis, they found that differentially expressed genes related to cell migration, skeletal system development, and bone mineralization were enriched within the labial alveolar bone tissues of the lower jaw. The Kyoto Encyclopedia of Genes and Genomes pathway enrichment analysis indicated that the focal adhesion (FA) pathway was upregulated, with focal adhesion kinase (FAK), a key signaling protein of the FA assembly, being highly expressed in the ABL + LM group. To validate their findings, they treated periosteal stem cells (PSCs), a group of stem cells that envelop the bone tissue, with an FAK inhibitor followed by exposure to ABL. The inhibition group showed poor proliferation and migration of PSCs, confirming that FAK activation was crucial to ABL-induced alveolar bone formation.
Prof. Yuan concludes by highlighting the potential applications of the study, “Our study presents a promising therapeutic approach for in situ alveolar bone augmentation via local ABL drug administration, which may prevent or repair the detrimental periodontal dehiscence.”
In summary, this study showcases a remarkably promising therapeutic approach for preventing and treating periodontal dehiscence, bringing significant benefits to ensuring safer orthodontic treatment.
***
Reference
Title of original paper: Local abaloparatide administration promotes in situ alveolar bone augmentation via FAK-mediated periosteal osteogenesis
Journal: International Journal of Oral Science
DOI: 10.1038/s41368-025-00392-6
About Sichuan University
Founded in 1896, Sichuan University comprises three former national universities: the former Chengdu University of Science and Technology, the former Sichuan University, and the former West China University of Medical Sciences. Today, it has evolved to become one of the largest universities in China, with a total of 49,146 students, of which 2,686 are international students. It consists of three campuses: Wangjiang, Huaxi, and Jiang'an, covering an area of 470 hectares and boasting 2.817 million square meters of floor space. Through research collaborations and joint academic programs with leading research universities from across the globe, it has established itself as a premier institute for education, research, and social impact.
Website: https://en.scu.edu.cn/
About Professor Quan Yuan from Sichuan University, China
Dr. Quan Yuan is a Professor in the Department of Oral Implantology, and the Vice Director of State Key Laboratory of Oral Diseases, Sichuan University, China. He earned his Doctor of Dental Surgery degree and pursued his postgraduate program in Oral Implantology at the West China School of Stomatology. His research focuses on oral implantology, periodontology, and bone regeneration. He has published 243 papers that have been cited more than 8,000 times. He also serves as the Vice Editor or editorial board member for eight scientific journals.
About Professor Yu Li from Sichuan University, China
Dr. Yu Li currently serves as a Professor in the Department of Orthodontics, Sichuan University, China. He obtained the Doctor of Dental Surgery degree from Sichuan University in 2009. His main research interests include orthodontics, orofacial orthopedics, biomechanics, and biomaterials. Over the years, he has published 99 papers that have been cited more than 3,000 times. In addition to being an active researcher, he serves as an Editor of the official orthodontics textbook for Chinese dental schools, and a committee member of the Chinese Orthodontic Society (COS).
Funding information
This work was supported by the National Natural Science Foundation of China (NSFC) (82371003) and the Elite Research Grant of the International Orthodontics Foundation 2022.
Yini Bao
International Journal of Oral Science
2885546461 ext.
ijos@scu.edu.cn
Visit us on social media:
X
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.